4 Unusual Signs of Sleep Apnea
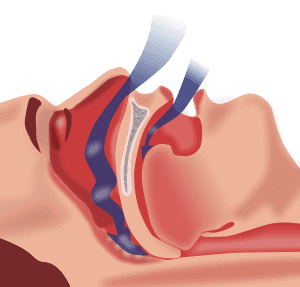
Sleep apnea is a problem affecting millions of Americans today. Left untreated, sleep apnea can wreak havoc on physical and mental health. From heart disease and stroke to depression and anxiety, the number of health problems caused or worsened by snoring and obstructive sleep apnea are virtually innumerable.
For this reason, treating sleep apnea as soon as you are aware you have it is essential to ensuring your ongoing well-being.
Most people are aware of the primary sign of obstructive sleep apnea: snoring. In fact, this is the primary symptom that people find bothersome and usually the one that ends up bringing them to their physician or healthcare provider for advice and treatment.
Other symptoms of sleep apnea that are commonly recognized are pauses in breathing while sleeping, tiredness regardless of the number of hours slept, and generalized fatigue.
However, there are many other signs of sleep apnea that are less common and often go unnoticed or unreported. Most of the time, people are unaware the physical signs they are having are related to sleep apnea at all. It is essential to be aware of the changes your body is facing in case they are related to sleep apnea or another health condition.
Below are the top four most unusual signs of sleep apnea that many people miss before their diagnosis.
Chapped Lips

Few people would think to make the connection between chapped lips and sleep apnea. Typically, people associate chapped lips with dry air and not much else. However, scientists have established a link between dry, chapped lips and sleep apnea.
According to some, the forced movement of air across the lips that is caused by sleep apnea is the reason so many people with the condition suffer from chapped lips. This is due to the dehydrating effects of continuous movement of air through the mouth.
Rather than slapping on some lip balm the next time you have chapped lips, you may want to consider treating your sleep apnea first to see if the dryness of your mouth improves.
Changes in Thinking, Memory, and Concentration
If you have difficulty remembering things or notice your memory is poorer than what it used to be, this may be a potential sign of sleep apnea.
Similarly, difficulty concentrating or paying attention to specific tasks is another little-known but important symptom of sleep apnea as well.
All these changes in the way you think and remember are related to the fact that sleep apnea dramatically impairs your ability to sleep through the night and get a good night’s rest. If you are not reaching the REM stage of sleep, then you are not getting enough time for your mind to recover, and your thinking will be adversely impacted as a result.
If you or your loved ones notice a decline in your memory or ability to concentrate on tasks for an extended period, it may be related to not having gotten enough restful sleep as a result of sleep apnea.
However, there is good news: if sleep apnea is the cause of your memory loss, loss of concentration, or other change in mentation, it is easily reversible with treatment of sleep apnea and the symptom of snoring.
Waking Up to Use Bathroom in The Night
One of the symptoms of sleep apnea that comes as a surprise to many people is nocturia, or frequently needing to urinate during the nighttime.
Usually, people associate this with bladder or prostate problems or have the belief that it is a natural part of aging. However, sleep apnea can cause the urge to void during the night as well.
As recent research shows, a type of hormone that causes increased urination is released when your body has to keep preventing you from stopping breathing during the night. This often happens in people with sleep apnea.
If your physician is concerned about your urinary frequency during sleeping hours, it is worth bringing up the potential for a sleep apnea diagnosis to him or her.
Mood Swings, Sadness, and Irritability
Science is clear: people with untreated sleep apnea have less sleep and a lower quality of sleep than those who do not.
If you are constantly tired due to waking up throughout the night, as people with sleep apnea are, it is natural that feeling fatigued, irritable, sad, and even hopeless will result. Treating the sleep apnea improves sleep duration and quality, which in turn eases these serious effects on mental health.
Final Thoughts
If you are experiencing one or more of these signs, it is a good idea to speak with your doctor or healthcare provider about the possibility of sleep apnea. This is especially true of you also snore or wake up often during the nighttime, or if your partner reports that you stop breathing periodically when you are sleeping.
If you have sleep apnea, you may need to use a device to stop snoring. These include devices to readjust your jaw, chin positioning straps, and anti-snoring pillows. Using these devices can alleviate symptoms of sleep apnea such as sadness, headaches, and memory loss, and help you get a restful night’s sleep.